¶ Introduction
Bi-level ventilators, also known by the trade name BiPAP®[1], are non-invasive ventilators that alternate between a high and low pressure to facilitate respiration.
Bi-level ventilators are capable of facilitating adequate respiration in an individual that has almost zero ability to breathe independently. However, in the case of ALS, spasticity (stiffness) of the diaphragm muscle may prevent sufficient respiration from occurring, even with the use of a bi-level machine that is configured to provide a great deal of support.
Bi-level ventilators are not strictly considered to be life-saving devices, however, it is possible for the user to be so dependent upon its function that they could require urgent medical care if it were to fail or if they were to lose access to it.

ResMed Stellar 150 bi-level ventilator with humidifier.
¶ Functionality
Many different bi-level ventilators exist in the market. Some have special features built into them, such as cough assistance.
Bi-level ventilators work in a number of different ways, depending on the model. The following are modes that the devices can operate in. Not all devices support all modes.
-
Spontaneous, whereby the device monitors pressure drops triggered by independent breathing, and then supplies air to the patient
-
Timed, whereby the device delivers a fixed amount of air based on set parameters
-
A combination of spontaneous and timed
Some ventilators have data acquisition functionality. Data is accessed either by attaching removable storage, such as a USB stick, or by transferring data over the Internet, using a modem connected to the ventilator. Proprietary software is used to interpret the data.
¶ Usage
¶ Acclimation
The feeling of a ventilator can be challenging to adjust to. Nighttime usage requires adapting to the feeling of the ventilation itself, along with the feeling of the mask, and the sound that the machine makes. Daytime usage presents fewer challenges in this regard.
One way to get used to using a ventilator is to use it while being distracted, such as by watching a movie.
¶ Schedule
Breathing difficulties are encountered progressively, similar to limb weakness. Early usage of a bi-level ventilator typically begins with occasional usage when breathing difficulties are being encountered. Often, these difficulties are most pronounced when lying down. As a result, overnight use tends to be the most common time when the ventilator first gets consistent use.
Follow the schedule recommended by the pulmonologist.
Usage of the ventilator will increase as breathing difficulties worsen. Daytime use on an as-needed basis typically follows a period of only using it overnight.
Eventually, the patient may need the ventilator constantly, except for brief periods such as speaking, eating, or maintaining oral hygiene.
¶ Masks and Fitment
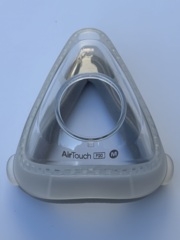
Masks come in different form factors. Selection of a mask type is typically based on comfort, and how it is being used, such as overnight or during the day.
Most models come with a small paper measurement tool, which is placed on the face. Markings on the measurement tool will indicate which size of that product is recommended. Some experimentation may be required to find an ideal fit.
Placing the mask at the correct place on the face before pulling the headgear over the head can make the process of fitting the mask and headgear easier.
¶ Power Supply
Most ventilators are equipped with an internal battery, so that they may run in the absence of an external electrical supply. These batteries vary in size; some may only allow the machine to run for an hour or two.
Have a plan for how to supply the ventilator with power in the case of a power outage.
The ventilator will trigger an alarm if external power is lost, and it needs to run on its internal battery. This alarm can be muted when running on the battery is intentional. Another alarm will sound when the internal battery is almost out of power.
¶ Placement of the Machine
The ventilator should be within reach of the user whenever possible.
The ventilator should always be placed at an elevation that is slightly lower than the user's head. The water reservoir in the machine may leak in some circumstances; having the user's head slightly higher reduces the risk of aspirating water.
The hose that connects the mask to the machine should be free of twists or kinks, and should be easy to move. When in bed, it should be possible for the user to lie in any sleeping position without the hose being put under any tension.
Leakage at the mask may occur if the hose becomes taught when lying in a certain position; in extreme circumstances, the mask may come right off.
¶ Humidification
Bi-level ventilators are often fitted with heated water humidifiers to increase comfort for the user. Distilled water is recommended, however, clean municipal water may be used temporarily.
Water that is not distilled may cause boiler scale (calcium deposits) to form inside the reservoir.
Avoid overfilling the water reservoir. An overfilled reservoir can cause water to travel through the air hose. Turn off the machine and decrease the water level if bubbling sounds are heard.
Empty the water reservoir before travelling with the device. If water from the reservoir were to splash inside of the ventilator, it could cause permanent damage to it.
¶ Maintenance
¶ Schedule
All parts of the ventilator between the water reservoir and the mask should be cleaned daily to prevent buildup of bacteria. The water reservoir, despite being very far away from the user's mouth is susceptible to accumulating significant amounts of bacteria.
The water reservoir, hose, mask, headgear, and inlet filter should be replaced per the manufacturer's recommendations.
¶ Method
¶ Mask cleaning
Most mask manufacturers recommend cleaning the mask using special wipes that are gentle on the materials that the mask is made of. These wipes are typically marketed as "CPAP wipes". The masks can also be rinsed with clean warm water.
¶ Hose cleaning
Hoses can be cleaned using tapwater and a small amount of antibacterial dish soap. It is important to rinse out all traces of dish soap as otherwise particles of it can enter the user's airway.
¶ Humidifier reservoir cleaning
Humidifier reservoirs can be cleaned using tapwater and a small amount of antibacterial dish soap. As with cleaning the hose, it is important to remove all traces of dish soap to prevent it from entering the user's airway.
Some humidifier reservoirs have a removable top that makes it easier to clean all internal surfaces. If present, remove the top. If an alternate top with a holding surface is provided, use it during the cleaning process.
¶ Common Problems
¶ Air leakage
Bi-level ventilators are designed to tolerate a modest amount of leakage in the hose and at the mask fitment interface. Achieving a perfect seal is not possible. However, excessive leakage will negatively affect operation. The ventilator will compensate for leakage by increasing the flow volume; this may produce a feeling of having one's face in a strong breeze. Breathing is uncomfortable in this circumstance and can be challenging. If the leak is extreme, inadequate flow of air into the lungs will result, and the machine will trigger an alarm.
Leakage is usually easy to hear and feel; checking for leaks and attempting to mitigate them is prudent, especially before going to the trouble of having the ventilator's settings changed.
Leakage may occur anywhere there is pressurized air between the ventilator outlet and the user's face. This includes:
- the mask, where it contacts the users's face
- either end of the hose, or a punctured section of the hose along its length
- cracks or holes in any part of the machine that is under pressure during operation, such as the humidification reservoir, if one is fitted
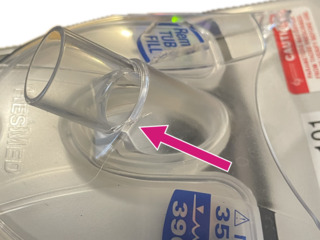
Bilevel humidifier enclosure showing a small crack. Air leakage is prevented only when manual pressure is applied to close the crack; leakage resumes immediately once the pressure is released. This part must be replaced.
Leakage at the mask interface can often be reduced by adjusting the headgear. While tightening the mask may intuitively seem to help, overtightening can crush the gasket against the user's face, potentially increasing leakage instead of reducing it.
Replacing the mask may be necessary if adjustment doesn’t resolve the issue. Over time, the mask gasket can wear out, preventing a proper seal.
If the mask continues to leak despite reasonable adjustment efforts, a different mask size or shape may need to be used.
¶ Dry mouth
Dry mouth can occur when using a ventilator if the nasal cavity is restricted. Consult a physician if dry mouth becomes a serious issue.
¶ Facial skin irritation
Dry or damaged skin can occur at the mask interface, or around the mouth. Use of a suitable moisturizer may work in some cases.
A ventilator whose water reservoir, hose, and mask are not regularly cleaned significantly increases the risk of infection due to the buildup of bacteria. The ventilator equipment should be cleaned daily to minimize this risk.
¶ Eye infection
Eye infection can be caused by significant leakage at the mask interface in the direction of the eyes. Eye infection can be prevented by keeping the equipment extremely clean, and adjusting the mask fitment interface to prevent leaks.
¶ Intestinal gas
A bi-level ventilator can generate sufficient pressure to force air past the esophageal sphincter, leading it into the stomach and eventually the intestines. This air is then released as flatulence. This phenomenon is known as aerophagia.
Essentially, the pressurized air from the ventilator will follow the path of least resistance. If there are restrictions or blockages in the nasal cavity or other parts of the airway, the air will divert into the digestive system instead.
Aerophagia can be managed by adjusting the ventilator settings, which should be done by a qualified professional.
¶ Communication difficulties
Speaking while wearing a mask is difficult. The listener may not be able to understand what is being said, unless it is being said loudly between in-breaths from the machine.
Products exist which amplify the speaker's voice through the mask so that they can be more easily understood.
A user with minimal respiratory difficulty may be able to remove the mask temporarily to speak. An alarm will be triggered if the mask is left off for a prolonged length of time while the machine is still running.
¶ Configuration
Bi-level ventilators have a number of different configuration parameters. Below are the fundamentals:
| Parameter | Description |
|---|---|
| IPAP (Inspiratory Positive Airway Pressure) | The pressure applied during inhalation; the higher of the two pressure levels. |
| EPAP (Expiratory Positive Airway Pressure) | The pressure during exhalation; the lower of the two pressure levels. |
| Rise Time | The time it takes for the ventilator to reach IPAP from EPAP. |
| Trigger Sensitivity | Determines how easily the ventilator detects patient effort. |
| Cycle Sensitivity | Controls the transition from inhalation to exhalation. |
| Backup Rate | The minimum number of breaths per minute delivered. |
| Leak Compensation | Adjusts for air leaks to maintain effective ventilation. |
The most frequently tuned configuration parameters are the IPAP and EPAP values. These are sometimes referred to colloquially as IPAP "over" or "on" EPAP. For example, a respiratory therapist may say that the device is configured to "16 on 5", which would be IPAP = 16 cm H2O and EPAP = 5 cm H2O.
Configuration parameters should only be determined by a qualified physician.
Changing the configuration parameters on a ventilator can sometimes be done over the phone by a caregiver or by the patient if they are able.
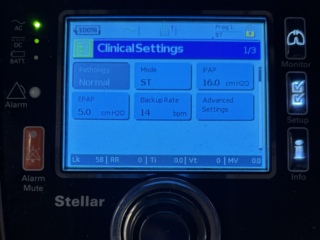
Clinical settings screen on a ResMed Stellar 150 bi-level ventilator.
¶ Further Considerations
Bi-level ventilators are often not available for sale to the general public; a ventilator must be prescribed by a physician.
Personal care assistants or other caregivers may require training before being allowed to even touch a ventilator.
Spare parts for ventilators, such as replacement masks, hoses, and water reservoirs may be hard to come by in some regions. It is wise to have a spare set of all of these items in case of accidental loss or breakage.
¶ See Also
- Lung Volume Recruitment Bags links to: Lung Volume Recruitment
- Mechanical Insufflator-Exsufflators a.k.a. Cough Assist
- Mouthpiece Ventilators